
Arthritis is an umbrella term that includes more than 100 related conditions. But two of the most common types, osteoarthritis and rheumatoid arthritis, are often confused, says Andrea Kane, a spokeswoman for the Arthritis Foundation. “A lot of people who have osteoarthritis are told by their doctors they have arthritis,’ she says. “And when anyone tries to make a distinction, they just hear ‘arthritis.’” But these two types of arthritis have different causes, symptoms and treatments.
Osteoarthritis
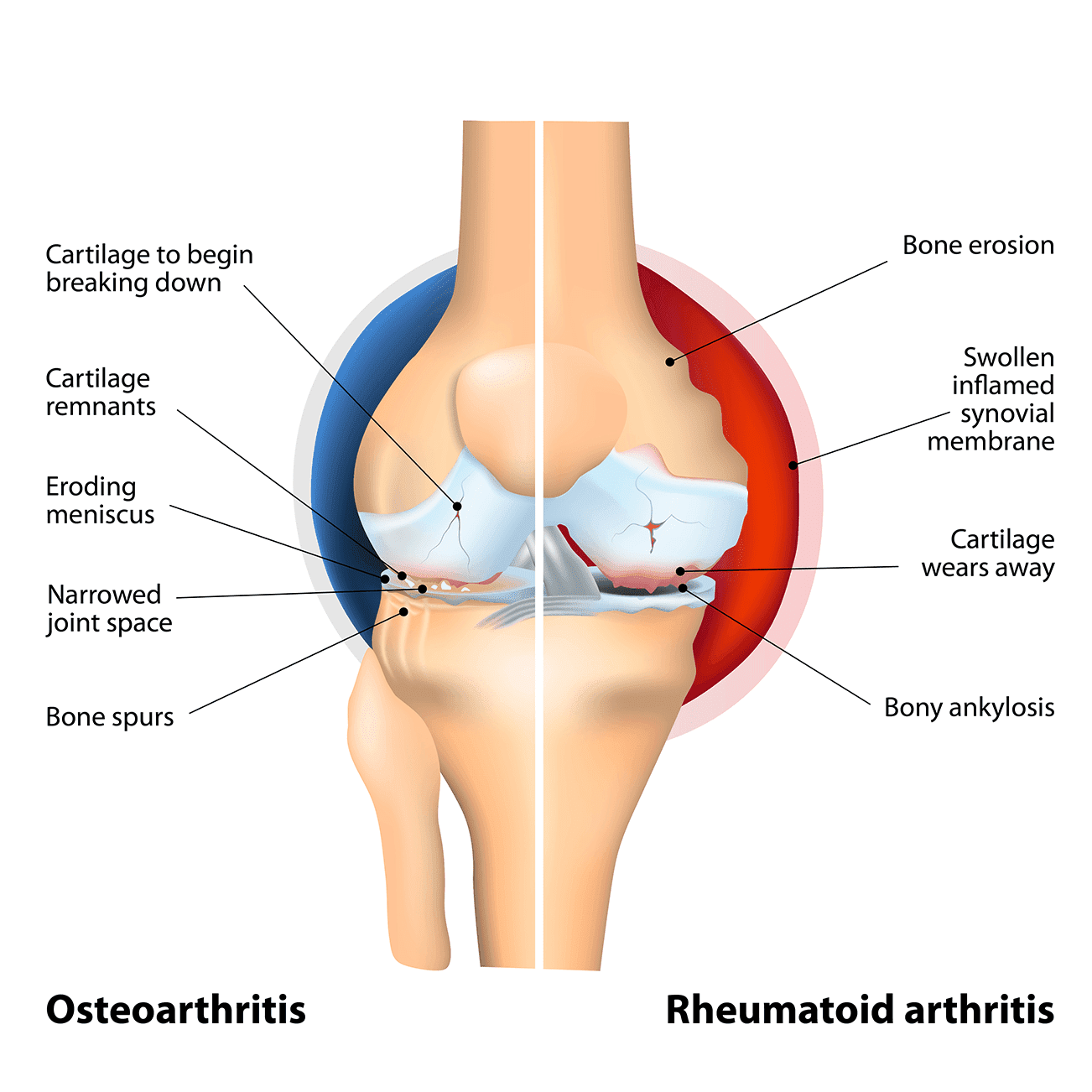
Osteoarthritis develops in joints that have been injured or overused. It affects more than 30 million people in the U.S. and often strikes the knees, hips or hands. Joint pain is the most common symptom of osteoarthritis.
"Osteoarthritis is a 'wear and tear arthritis,'" explains Dr. Vandit Sardana, a board-certified and fellowship-trained orthopedic surgeon with Beaufort Memorial Orthopaedic Specialists. "It requires strengthening of muscles with physical therapy to offload pressure on the joint; injections such as cortisone, hyaluronic acid or stem cells; and anti-inflammatory medications such as Advil®, Aleve®, etc."
Rheumatoid Arthritis
Rheumatoid arthritis develops when the immune system attacks joints and organs, which causes painful swelling. It’s less common than osteoarthritis, affecting about 1.5 million adults in the U.S.
“Rheumatoid arthritis usually affects multiple joints and needs medical attention with disease modifying anti-rheumatic drugs (DMARDS) to keep it in remission," says Dr. Sardana. "There are various blood tests combined with a thorough history and physical exam that can help diagnose rheumatoid arthritis."
Both conditions require treatment, which can include physical therapy, medications and surgery. If you have joint pain that lasts six weeks or longer, morning stiffness that lasts at least 30 minutes, or pain in the same joints on both sides of your body, it’s a good idea to speak to your doctor.
"Once the joints are eroded, whether from osteoarthritis or rheumatoid arthritis, the treatment is joint replacement surgery," explains Dr. Sardana. "Your physician has to be careful in diagnosing the type of arthritis, however, as that diagnosis will guide the type of prosthetic used in your joint replacement so that you attain stability and a well-balanced joint.”
Managing Chronic Pain from Arthritis
Medication
Your physician can recommend prescription and over-the-counter medications to help control inflammation and pain.
Weight Management and Physical Activity
Excess weight puts more pressure on the weight-bearing joints and increases pain. Fatty tissue also increases hormones related to inflammation.
In addition to helping control weight, activities like walking, water aerobics and yoga can help reduce joint pain and improve flexibility, balance and strength. If you are new to exercise, talk to your doctor or physical therapist to find out what may be best for you.
Positive Attitude
Many people with chronic arthritis pain find that a positive attitude can significantly boost their ability to cope with pain. Finding ways to keep your mind off the pain can help. Do things you enjoy – like a hobby or spending time with family and friends – to keep your spirits high. Ask your doctor about how hypnosis, meditation and breathing techniques can help you ease your pain.
For more information about chronic pain and how to manage it, use the Arthritis Foundation's Breaking the Pain Chain® toolkit.
Options for Joint Pain
Attend the next Solving Hip & Knee Pain class to discuss your symptoms and learn about all of the treatment options. Or set an appointment with a board-certified orthopedic specialist.

