After having a stroke nine years ago, Barbara Ottaway gave up a bad habit that had dogged her most of her life — she stopped smoking.
After having a stroke nine years ago, Barbara Ottaway gave up a bad habit that had dogged her most of her life — she stopped smoking.
“I wasn’t a heavy smoker,” the 72-year-old Lady’s Island resident says. “I only smoked three cigarettes a day — mostly during breaks at work. But the stroke was a wake-up call.”
Then last fall, she developed a persistent sore throat and what felt like a lump on the back of her tongue. Having successfully kicked her tobacco habit, she didn’t think anything of it and never sought medical attention.
 “I grew up poor and we didn’t go to the doctor or dentist,” Ottaway says. “The first time I went to the doctor was when I had my baby at age 34.”
“I grew up poor and we didn’t go to the doctor or dentist,” Ottaway says. “The first time I went to the doctor was when I had my baby at age 34.”
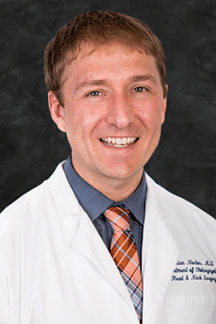
But by December, the lump had grown so large, she was having trouble swallowing. She ended up in the Beaufort Memorial Pratt Emergency Center where she was treated for her symptoms and referred to Beaufort Memorial ear, nose and throat specialist Dr. Julien Norton. After examining her throat, he ordered CT and PET scans of her neck. A biopsy confirmed it was Stage IVA oral squamous cell carcinoma, a type of oropharyngeal cancer. The cancer had invaded the back third of her tongue, which starts in the throat, and spread to lymph nodes in her neck.
An Unexpected Diagnosis
A Beaufort Memorial medical oncologist broke the news to her Dec. 21.
“It was the furthest thing from my mind,” Ottaway says of the cancer diagnosis. “But I was remarkably calm. I didn’t cry. I didn’t ask why. I just figured that either I would be taken home to heaven or I’d be cured.”
As it turned out, the cancer was not related to her prior smoking habit. It was caused by the human papillomavirus (HPV).
Read More: Protection Against HPV
“Oropharyngeal cancer is not as common as breast or lung cancer, but it’s rising,” Dr. Newberry says. “It used to be a lifestyle cancer caused by smoking and drinking. However in recent years, we’ve seen a shift to patients testing positive for papillomaviruses.”
The treatment strategy for oral cancer focuses on preserving the tongue. Because Ottaway’s tumor had not spread outside the tongue and neck area, surgery was not required. Instead, her Beaufort Memorial cancer team recommended an aggressive regimen of both chemotherapy and radiation to battle the advanced cancer.
 “One of the more difficult side effects from radiation to the mouth, throat and neck is that it affects the salivary glands,” says Dr. Jonathan Briggs, radiation oncologist at Beaufort Memorial. “Saliva is what cleanses the mouth and teeth, so if the salivary glands aren’t working properly and you have a cavity, you risk getting an infection in the bone, which can be very, very painful.”
“One of the more difficult side effects from radiation to the mouth, throat and neck is that it affects the salivary glands,” says Dr. Jonathan Briggs, radiation oncologist at Beaufort Memorial. “Saliva is what cleanses the mouth and teeth, so if the salivary glands aren’t working properly and you have a cavity, you risk getting an infection in the bone, which can be very, very painful.”
Before starting chemoradiation therapy, Dr. Briggs advised Ottaway to see a dentist.
“I hadn’t been to a dentist in 20 years,” Ottaway says. “I had nine cavities.”
After the dental work was completed, a feeding tube had to be inserted into her stomach. Ottaway’s radiation treatment would affect her ability to eat.
Six Weeks of Treatment
 On Jan. 20, she began the prescribed six-week course of treatment, which included weekly chemotherapy and radiation five days a week. She received the chemo at Beaufort Memorial Chemotherapy and Infusion Services and radiation treatment at the Keyserling Cancer Center on the main hospital campus.
On Jan. 20, she began the prescribed six-week course of treatment, which included weekly chemotherapy and radiation five days a week. She received the chemo at Beaufort Memorial Chemotherapy and Infusion Services and radiation treatment at the Keyserling Cancer Center on the main hospital campus.
“I felt so blessed to be able to get the treatment so close to my home,” Ottaway says. “The doctors at Beaufort Memorial were phenomenal. They see the horrors of cancer every day, and though they are realists, they try to lift you up.”
Read More: Possible Cancer Symptoms Women Can’t Afford to Miss
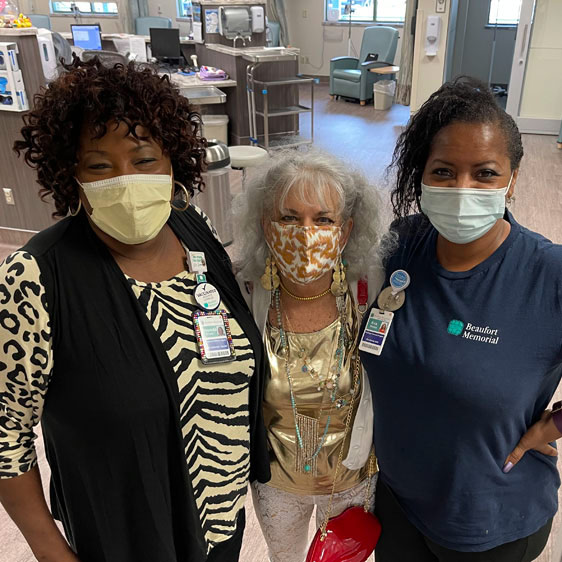
 Ottaway was just as impressed with the staff at the infusion and cancer centers.
Ottaway was just as impressed with the staff at the infusion and cancer centers.
“Everyone was so kind and considerate,” she says. “They are the most incredible, wonderful people on the face of the earth.”
While not painful, radiation in the mouth can be difficult. Ottaway experienced dry mouth, soreness swallowing, fatigue and loss of taste.
“I didn’t throw up or lose my hair, but everything tasted like plastic,” she says. “I looked awful and had no energy, so I would go home and get in bed after each treatment.”
Success on Two Fronts
 Three months after Ottoway’s chemoradiation therapy was complete, she had imaging tests to evaluate her prognosis.
Three months after Ottoway’s chemoradiation therapy was complete, she had imaging tests to evaluate her prognosis.
“The PET scan showed no cancer anywhere in her body,” Dr. Briggs says. “It was a successful treatment.”
To ensure she obtained sufficient nutrition, she was kept on the feeding tube until the beginning of June. The restrictive diet came with a benefit. Since September, she has lost 65 pounds.
A self-described sugaraholic, Ottaway was obese when she started the ordeal. Now that she has lost the weight, she plans to keep it off by maintaining a healthy diet.
“I’m consuming an eighth of the food I used to put in my body,” Ottaway says. “I’m at the weight I was in middle school. I threw away nine bags of plus-size clothes and now fit in size 4 jeans!”
If it’s been more than a year since you had a wellness visit with your primary care provider, schedule a visit now to ensure you are up to date on all of your health screenings.
Don’t have a primary care provider? Find one accepting new patients.